From Tension to Regulation
From Tension to Regulation: Understanding the Stress Cascade
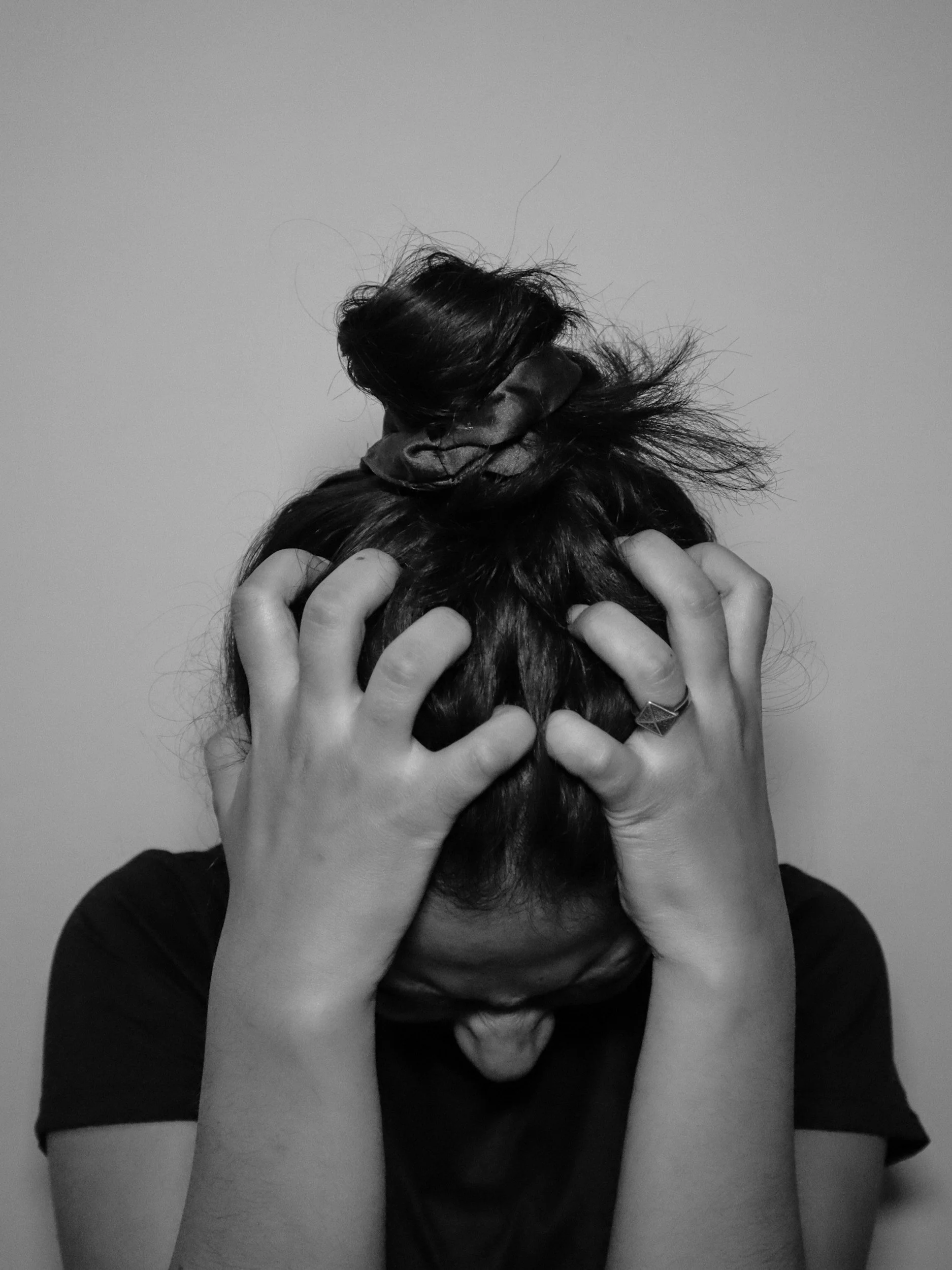
We all experience stress. It is a normal and even necessary part of being human. But when stress becomes constant, the body forgets how to return to baseline. Over time, this chronic “on” state begins to change our biology, affecting everything from hormones and digestion to sleep, inflammation, and pain.
Let’s explore what actually happens inside the body when we live in a constant state of stress, and how we can begin to regulate again.
The HPA Axis: Your Body’s Stress Command Center
When the brain perceives stress, whether it is a work deadline, poor sleep, chronic pain, or ongoing worry, the hypothalamic pituitary adrenal axis, known as the HPA axis, is activated.
The hypothalamus signals the pituitary gland, which then signals the adrenal glands to release cortisol and adrenaline. These hormones prepare the body for fight or flight by increasing heart rate, blood sugar, and alertness, while suppressing functions deemed non essential for survival, such as digestion, reproduction, and repair.
This short term response is helpful in emergencies. But when the signal never shuts off, cortisol remains elevated and the body stays in survival mode. This is known as sympathetic dominance.
When Survival Becomes Chronic
Chronic activation of the HPA axis keeps the body locked in a high alert state. Over time, this can lead to several patterns of dysfunction.
Adrenal dysregulation occurs when cortisol rhythms flatten. Cortisol may be too high at night, contributing to insomnia, and too low in the morning, leading to fatigue and brain fog.
Thyroid suppression can occur as the body down regulates metabolism in an attempt to conserve energy. This often shows up as cold intolerance, sluggish digestion, and weight gain.
Sex hormone imbalances develop because cortisol and sex hormones share the same precursors. Prolonged stress pulls resources away from progesterone and DHEA production, contributing to PMS, irregular cycles, and mood changes.
Digestive slowdown is also common. Stomach acid and enzyme output decrease, impairing nutrient absorption and gut motility.
This hormonal dysregulation creates a ripple effect across nearly every system in the body.
Stress and Digestion: The Gut Brain Loop
In a parasympathetic, rest and digest state, the gut thrives. It secretes enzymes, breaks down food efficiently, and communicates clearly with the brain through the vagus nerve.
Under chronic stress, several things shift.
Vagal tone weakens, impairing communication between the brain and the gut. Gut permeability increases, allowing undigested particles and toxins to enter the bloodstream. The immune system becomes hyper reactive, triggering systemic inflammation. Gut bacteria shift toward stress loving species, further disrupting immune balance and mood regulation.
Because nearly 95 percent of serotonin is produced in the gut, stress related dysbiosis directly impacts mental health. This often shows up as anxiety, irritability, and sleep disturbances.
The Blood Sugar Connection
One of cortisol’s primary roles is to mobilize glucose for energy. When cortisol is chronically elevated, blood sugar remains high and insulin is forced to work overtime.
Over time, this can lead to insulin resistance, frequent energy crashes and cravings, and increased production of inflammatory cytokines that fuel pain and fatigue.
Blood sugar swings also worsen anxiety and mood instability, creating a feedback loop that keeps the HPA axis activated.
Sleep, Recovery, and the Nighttime Reset
Cortisol and melatonin follow an inverse rhythm. Cortisol should be highest in the morning and lowest at night, while melatonin rises in the evening to promote sleep.
Chronic stress flattens this rhythm, often causing difficulty falling or staying asleep, nighttime awakenings commonly between two and four in the morning, and grogginess upon waking with unrefreshing sleep.
Without restorative sleep, the body cannot clear inflammatory waste through the glymphatic system, repair tissues, or reset hormonal balance. This perpetuates fatigue, inflammation, and dysregulation.
From Hormones to Inflammation and Pain
Digestion, blood sugar regulation, sleep, and immune signaling are deeply interconnected. Elevated cortisol and insulin promote the release of inflammatory cytokines, which sensitize pain receptors, stiffen fascia and connective tissue, and impair blood flow and tissue oxygenation.
This is why stress often manifests as chronic neck or back pain, headaches, jaw tension, or muscle stiffness, even in the absence of physical injury.
Regular bodywork, fascia release, and craniosacral therapy help interrupt this loop by calming the HPA axis, improving vagal tone, and re educating the body’s perception of safety.
The Statistics Tell the Story
Nearly 77 percent of Americans report regular physical symptoms of stress.
Eighty percent of people live primarily in a sympathetic state, meaning their nervous systems rarely down regulate into rest and digest.
Chronic stress is linked to 75 to 90 percent of primary care visits, often presenting as fatigue, digestive issues, pain, anxiety, or insomnia.
Our nervous systems were never designed to live in constant fight or flight.
Regulating the Stress Response: Returning Home to the Body
You cannot eliminate all stress, but you can retrain your body to respond differently. Here are a few ways to begin.
Bodywork and craniosacral therapy help calm the HPA axis and restore circulation.
Breathwork, especially long exhales, activates the vagus nerve and lowers cortisol.
Natural light exposure helps regulate circadian rhythm and cortisol timing.
Protein and fiber rich meals stabilize blood sugar and reduce cortisol spikes.
A consistent bedtime aligns hormone rhythms for repair and restoration.
Gentle movement such as walking, yoga, or stretching releases muscle tension and supports lymph flow.
Coming Home to Safety
Stress itself is not the villain. It is a messenger, the body’s way of saying something needs attention. The real problem begins when we stop listening.
When the pace of life keeps us in constant motion, the body never receives the signal that the danger has passed. Over time, that unrelenting state of activation becomes the norm. Tight shoulders, shallow breathing, a restless mind, a gut that cannot quite settle.
We begin to believe this is simply what it feels like to be human. But it is not.
Every system in the body, digestive, hormonal, immune, cardiovascular, depends on one fundamental state: safety. Without it, the body cannot prioritize healing, growth, or connection. Chronic activation burns through nutrients, weakens the gut barrier, increases inflammation, and diminishes our capacity to repair, digest, and rest.
This is where regulation begins.
When you intentionally create safety through touch, nourishment, breath, stillness, and rest, the body starts to remember. The HPA axis calms, cortisol finds balance, and the parasympathetic nervous system returns as the baseline state.
Moments of restoration are not indulgent. They are essential.
Each time you slow down, breathe deeply, receive bodywork, or eat a nourishing meal without distraction, you are telling your body:
You are safe now.
You can rest.
You can heal.
With care,
Mandi